
ЗАЩО?
Да висиш надолу с главата 7 минути на ден?
Страдате от болки в гърба или ви мъчи постоянна болка в кръста?
Имате нужда от упражнения при болки в гърба или в кръста?
Търсите ефикасно лечение на дискова херния, дископатия или стеноза?
Препоръчани са ви упражнения при дискова херния или дископатия?
Не премахвайте само симптомите, а атакувайте източника на болката! Ние имаме решение за вашия проблем, при това с възможност за избор!
EMBER 03 PREMIUM
Лежанката EMBER 03 Premium е проектирана както за професионална употреба в рехабилитационни центрове и фитнес зали, така и за домашна употреба.
- Ергономично проектирана с извита облегалка.
- Има удобна възглавница за по-добра опора на врата Ви по време на инверсия.
- Максимално тегло на ползвателя: 150 кг.
- Възможност за наклон под ъгъл 150 градуса, както и под наклон 180 градуса (глава на пода)
- Предвидена е възможност за регулиране ъгъла на наклона в три позиции чрез метален ограничител.
- Преди употреба задължително настройте лежанката спрямо Вашата височина (до 198 см.)
ТЕХНИЧЕСКА ХАРАКТЕРИСТИКА
- Tип задвижване: механично
- Максимално тегло на потребителя: 150 кг
- Максимална височина на потребителя: 198 см
- Особености: сгъваем дизайн, регулиране на височината, регулиране на глезена, регулиране на ъгъла на наклон
- Цвят на рамката: черен
- Цвят на тапицерията: черен
- Дължина: 130 см
- Ширина: 79 см
- Височина: 152 см
- Тегло: 35 кг
- Размери на опаковката: 146 см х 68 см х 24 см
ПОЛЗИ
- Премахване на временни и облекчаване на хронични болки в гърба.
- Превенция и третиране на стреса, мускулното напрежение и физическата умора.
- Подобряване на кръвооросяването и притока на кислород към мозъка.
- Превенция и облекчаване на болки, свързани с разширени вени.
- Подобряване на естествената позиция на тялото.
- Укрепване на лигаментния апарат.
- Ускоряване пречистването на кръвта и лимфната течност.
- Подобряване на гъвкавостта на тялото.
- Намаляване задържането на вода в краката и глезените.
БЕЗОПАСНОСТ
При правилно монтиране и използване в съответствие с препоръките на производителя, инверсната лежанка е напълно безопасна за здрави хора, които я използват за физически упражнения и превенция.
- Високо качество и издръжливост на изходните материали.
- Надеждна конструкция и свързващи елементи.
- Интелигентен функционален дизайн, гарантиращ безпроблемно изпозлване.
- Отлични резултати от тестването на продукта за безопасност по време на употреба.
Употребата на инверсна лежанка не се препоръчва при хора, страдащи от следните заболявания и състояния:
- Високо кръвно налягане
- Сърдечно-съдови заболявания
- Импланти в тялото
- Инфекции на средното ухо
- Бременност
- Костна слабост (остеопороза)
- Скорошни или не излекувани фрактури
- Костни импланти
- Хирургически имплантирани ортопедични подложки
- Употреба на антикоагуланти (вкл. високи дози аспирин)
- Възпаление на средното ухо
- Прекомерно затлъстяване
- Бременност
- Хиатална херния
- Вентрална херния
- Глаукома
- Отлепяне на ретината
- Конюнктивит
- Високо кръвно налягане
- Свръх напрегнатост
- Сърдечни проблеми или смущения в кръвообращението
- Травма на гръбначния стълб
- Церебрална склероза
- Остро възпаление на ставите
- Скорошен инсулт или временен исхемичен пристъп
Лежанка EMBER 03 PREMIUM
Ember 03 Premium комбинира подобрен ергономичен дизайн с висока издръжливост и сертифицирана безопасност - за да можете да отговорите на болките в кръста и гърба по възможно най-ефективния, неинвазивен начин.
Моделът е разработен за интензивна професионална употреба във фитнес зали, рехабилитационни центрове, домакинства с много членове или офис сгради със специални кътове за здраве и отдих.
Тя е стабилна, лесна за монтиране и гарантира успешна дългосрочна употреба както с цел превенция, така и с цел контрол върху различни хронични заболявания на опорно-двигателния апарат.
100% сертифицирана безопасност
Инверсната лежанка Ember 03 Premium има индивидуални TUV и SGS сертификати за качество и безопасност, които гарантират:
- Високо качество и издръжливост на изходните материали.
- Надеждна конструкция и свързващи елементи.
- Интелигентен функционален дизайн, гарантиращ безпроблемно изпозлване.
- Отлични резултати от тестването на продукта за безопасност по време на употреба.
Употреба на лежанка EMBER 03 Premium при 150 градуса наклон
EMBER 03 PREMIUM
Основни характеристики
Ember 03 Premium събира в себе си целия досегашен опит и добри примери от индустрията, като ги обогатява с допълнителни иновации и устойчивост:

Извита облегалка с ергономична форма за максимална декомпресия.

Допълнителна възглавница за подкрепа и комфорт в областта на врата.

Поддържане на максимално тегло до 150кг. и максимална височина до 198см.

Три лесно регулируеми позиции на наклона.
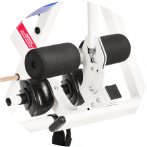
EMBER 11 LIGHT
Олекотената лежанката EMBER 11 LIGHT е предназначена за домашна употреба.
С тегло от само 23 киограма тя е идеалният уред за Вашето жилище.
- Лесно се сгъва и не заема много място в дома Ви
- Ергономично проектирана с извита облегалка.
- Има удобна възглавница за по-добра опора на врата ви по време на инверсия.
- Максимално тегло на ползвателя: 150 кг.
- Възможност за наклон под ъгъл 150 градуса, както и под наклон 180 градуса (глава на пода)
- Предвидена е възможност за регулиране ъгъла на наклона в три позиции чрез метален ограничител.
- Преди употреба задължително настройте лежанката спрямо Вашата височина (до 198 см.)
ТЕХНИЧЕСКА ХАРАКТЕРИСТИКА
- Tип задвижване: механично
- Максимално тегло на потребителя: 150 кг
- Максимална височина на потребителя: 198 см
- Особености: сгъваем дизайн, регулиране на височината, регулиране на глезена, регулиране на ъгъла на наклон
- Цвят на рамката: бял
- Цвят на тапицерията: син
- Дължина: 118 см
- Ширина: 72 см
- Височина: 144 см
- Тегло: 23 кг
- Размери на опаковката: 129 см х 77 см х 15 см
ПОЛЗИ
- Превенция на болки в гърба вследствие на претоварване или обездвижване
- Облекчаване на хронични болки в гърба, кръста, таза, раменете и врата.
- Подобряване на кръвообращението в тялото.
- Увеличаване на притока на кислород към мозъка.
- Редуциране на физическата преумора и психо-емоционалния стрес.
- Облекчаване на болки от разширени вени.
- Подобряване на процеса на пречистване на кръвта и лимфата.
- Укрепване на лигаментния апарат.
- Изправяне на стойката.
- Подобряване на гъвкавостта.
- Редуциране на задържаните течности в краката и глезените.
- Редуциране на ефектите от гравитационно предизвиканото стареене.
БЕЗОПАСНОСТ
Лежанката EMBER 11 LIGHT е напълно безопасна за здрави хора, които я използват за физически упражнения и превенция. За целта е необходимо единствено да я монтирате и използвате според инструкциите на производителя.
Инверсионната терапия не се препоръчва при високо кръвно налягане, сърдечно-съдови заболявания, глаукома, отлепване на ретината, фрактури, херния, импланти в тялото, инфекции на средното ухо и периода на бременността.
Ако страдате от каквото и да е диагностицирано хронично заболяване - включително и на опорно-двигателния апарат - употребата на уреди, терапии и медикаменти следва да бъде предварително обсъдена с Вашия лекар.
Употребата на инверсна лежанка не се препоръчва при хора, страдащи от следните заболявания и състояния:
- Високо кръвно налягане
- Сърдечно-съдови заболявания
- Импланти в тялото
- Инфекции на средното ухо
- Бременност
- Костна слабост (остеопороза)
- Скорошни или не излекувани фрактури
- Костни импланти
- Хирургически имплантирани ортопедични подложки
- Употреба на антикоагуланти (вкл. високи дози аспирин)
- Възпаление на средното ухо
- Прекомерно затлъстяване
- Бременност
- Хиатална херния
- Вентрална херния
- Глаукома
- Отлепяне на ретината
- Конюнктивит
- Високо кръвно налягане
- Свръх напрегнатост
- Сърдечни проблеми или смущения в кръвообращението
- Травма на гръбначния стълб
- Церебрална склероза
- Остро възпаление на ставите
- Скорошен инсулт или временен исхемичен пристъп
Лежанка EMBER 11 LIGHT
EMBER 11 LIGHT е сертифициран продукт, пригоден специално за употреба в домашни условия.
Лежанката предлага лесен и достъпен начин да обръщате тялото си под различни ъгли и да декомпресирате гръбнака си ефективно - без да напускате дома си, без да губите време и без да пилеете средства.
За да усетите ефектите от EMBER 11 LIGHT е достатъчно да използвате уреда няколко пъти седмично по няколко минути. На него можете да практикувате както пасивно разтягане и релакс, така и активни физически упражнения.

Основни характеристики
Инверсната лежанка EMBER 11 LIGHT е подходяща за използване както с цел превенция, така и с цел подобряване на състоянието при различни диагностицирани състояния на опорно-двигателния апарат.
Нейният интелигентен съвременен дизайн съчетава максимално удобство с лекота и 100% безопасност.
Основните технически характеристики на модела включват:

Извита облегалка, следваща ергономичната форма на гръбначния стълб.

Допълнителна подкрепа в областта на раменете и врата.

Наклон под три възможни ъгъла, включително и 180 градуса - изцяло преобърнато положение.

Поддържане на максимално тегло до 150кг. и максимална височина до 198см.

Лесно сгъване до компактни размери, подходящи за съхранение в дома.

Лесна регулация и стабилна фиксация на позициите само с няколко движения.
Лесна и удобна употреба в домашни условия
Теглото на EMBER 11 LIGHT е едва 23кг. - оптималното за постигане на отлична стабилност в комбинация с улеснена ежедневна употреба, пренасяне и складиране.
Моделът се сглобява еднократно, след което може лесно да се сгъва и прибира на удобно място, за да не заема излишно пространство.
В комплекта са включени както всички необходими инструменти за сглобяването на лежанката, така и подробни видео инструкции стъпка по стъпка.
Употреба на лежанка EMBER 11 LIGHT при 150 градуса наклон
Инверсните лежанки са помогнали на милиони да намерят естествено облекчение на своите болки!
Ако отделяте само няколко минути дневно за тренировки ще постигнете няколко сигурни резултата:
- Ефективно лечение на болките в кръста и гърба, успешна борба с дископатията, дисковата херния и стенозата.
Използването на лежанката отпуска мускулите, помага за обновяването на дисковете и ставите, премахва напрежението в гърба и кръста. -
Намаляване на стреса.
Упражненията с инверсната лежанка Ember освобождават напрежението в кръста и гърба. -
Увеличаване на гъвкавосттa.
Ежедневното използване на лежанката ще подобри физическата Ви форма за активен и здравословен начин на живот. -
Изграждане на силна основна мускулатура.
Подсилва основните мускули с упражнения в обърнато наопаки положение на тялото. -
Инверсната лежанка е полезна при:
Болки в кръста, болки в гърба, дископатия и дискова херния.

ЛЕКАРИТЕ ЗА ЛЕЧЕНИЕТО С ИНВЕРСНИ ЛЕЖАНКИ
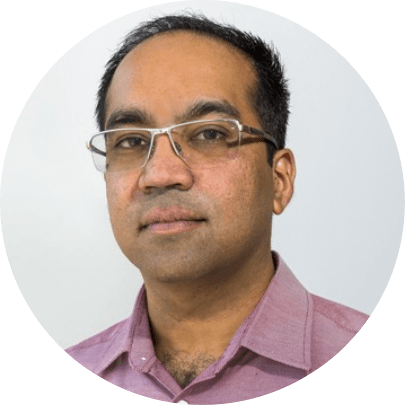
Д-р Джимша Джеймс
ОРТОПЕД
Инверсните лежанки не са нещо ново в полето на ортопедията и травматологията. Напротив - инверсната терапия се прилага широко в професионалната практика като един от най-достъпните и дългосрочни неинвазивни методи за облекчаване на болки в гърба, възникнали вследствие както на неправилен начин на живот, така и някои специфични заболявания на опорно-двигателния апарат.
Приветствам идеята инверсията да стане по-широко достъпна за масовия потребител извън рехабилитационните центрове. Вярвам, че правилната и регулярна употреба на лежанките за преобръщане на тялото може да служи еднакво добре за превенцията на потенциални проблеми - поле, в което все още имаме още много какво да постигнем като общество.
В моята практика, инверсията доказано постига значително редуциране на болката, свързана с мускулно напрежение, неправилна стойка, тежък физически труд, дископатия и дискова херния. Комбинирана със здравословни навици за живеене и физическа активност, тя определено може да изиграе немалка роля в здравето на костите, ставите, мускулите и тъканите.
Надявам се повече хора да преоткрият лесния начин да живеят добре, а именно - да обръщат нужното внимание на тялото си, преди нещата да ескалират и да се налагат инвазивни интервенции. Инверсните лежанки са лесен и достъпен начин това да стане факт, и то от комфорта на дома.
КОМПАКТЕН РАЗМЕР

- Компактна
- Лесна за употреба
- Създадена да помага
Инверсната лежанка е уредът, без който не можете!

ЛЕСНО ЗА УПОТРЕБА
ПРОСТО СЛЕДВАЙ ТРИТЕ СТЪПКИ

1. НАСТРОЙ ВИСОЧИНАТА

2. ЗАКЛЮЧИ

3. НАКЛОНИ СЕ И СИ ПОЧИНИ
КАКВО ПРЕДСТАВЛЯВА ИНВЕРСНАТА ЛЕЖАНКА?
Инверсионната лежанка е вид иновативно устройство за упражнения, разтягане и спортуване, което използва силата на земната гравитация за намаляване на натиска върху гръбначния стълб, който с времето се компресира. Базирайки се на концепцията за разсейване на компресията, инверсионната терапия използва собственото ви тегло и естествената гравитация, за да намали натоварването в гръбнака, гърба и различните мускулни групи.
Конструкцията на този изключителен инструмент за разтягане е доста опростена и включва стабилна стоманена стойка, върху която е поставена удобна маса, която може да се върти във всички посоки и под различни ъгли. Мултифункционалната лежанка може да се използва в домашни условия и упражненията на нея няма да Ви затруднят никак.

За кого са предназначени лежанките?
От инверсионната терапия, която предоставят упражненията на този изключителен инструмент за разтягане могат да се възползват хора от всякакви възрастови групи.

- Лежанките са предназначени за хора, които страдат от заболявания като дискова херния, болки в гърба, в кръста, стеноза, гръбначни изкривявания и други гръбначни заболявания.
- Полезни са и за хора, които просто искат да се отърсят от стреса и се нуждаят от малко “висене”, за да се почувстват отново във форма.
- От полза са и за активно спортуващите. С помощта на инверсната лежанка лесно могат да следват своя режим на тренировка, без значение дали това е динамична тренировка на лежанката или тренировка без усилие.
Как се правят упражнения на инверсна лежанка?
За да използвате инверсионната лежанка е необходимо просто да се облегнете и отпуснете на нея и да поставите краката си на удобната стойка. Отпуснете се и оставете гравитацията да свърши работата си. Можете просто да “висите” с главата надолу, да правите различни упражнения, да се люлеете или да я наклоните под друг ъгъл.
Ъглите на наклон, които можете да зададете са 20, 40, 60 или пълно преобръщане на тялото, а времето, през което е препоръчително тялото ви да остане под избрания ъгъл е до 15 минути.
Използването на инверсна лежанка Ember само по седем минути дневно например е повече от достатъчно, за да почувствате облекчение в гръбнака и кръста и да намалите натоварването във всички мускулни групи.


След колко време идва ефектът от инверсионната терапия?
Хората, които използват комбинираната лежанка за разтягане и спортуване споделят, че още след първия опит усещат намаляване на болките. Трениращите от 5 до 7 минути два - три пъти седмично на инверсна лежанка пък споделят, че само след месец са открили своето лечение на болките и могат не само да се движат нормално, но и да се върнат към любимите си занимания.
Как помагат лежанките за лечение и разтягане?
Инверсионната терапия е предназначена да противодейства на ефектите на гравитацията, които влияят върху телата ни. Гравитацията дърпа органите, мускулите и ставите надолу, компресирайки ги към гръбначния стълб.
С течение на времето и годините, които натрупваме, тази гравитационно причинена компресия може да доведе до поява на дискова херния, болки в горната част на тялото, в гръбнака и други заболявания с подобна симптоматика.
Упражненията с лежанките на Ember облекчават налягането в гръбначния стълб и увеличават пространството между прешлените, което помага за лечение на болките в гърба и кръста, облекчаване състоянието при дискова херния и други.
Освен при лечение на заболявания на опорно - двигателния апарат, инверсионната терапия е полезна, защото:
- Намалява стреса
- Повишава гъвкавостта
- Подобрява кръвообръщението
- Отпуска напрегнатите мускули
- Намалява налягането на нервите
- Рехидратира дисковете
- Повишава тонуса
Защо инверсни лежанки Ember?
Инверсните регулируеми лежанки Ember се произвеждат от 1981 година и се ползват с репутация на едни от най-качествените и иновативни лежанки за разтягане и спортуване за домашно ползване, които се предлагат на пазара. Лежанките на Ember се изработват от висококачествени материали и са единствените, на които сертифициращата лаборатория Underwriter's Laboratories е издала сертификат за качество и безопасност UL 1647.
Освен, че са качествени, Ember лежанките предлагат редица специализирани функции като:


- Автоматично заключващи се панти за предотвратяване на инциденти по време на разтягане или упражнения
- Специални ролкови лагери предотвратяващи скърцането
- Автомати, които позволяват на лежанката да се заключи при пълно преобръщане на тялото
- Възможност за персонализиране
- Всяка инверсна лежанка Ember се предлага и с диск с полезни упражнения, които могат да ви помогнат да се справите с проблемите в кръста, гърба и мускулите.
Отзиви от клиенти
Обичам фитнеса и всичко свързано с него, от години се занимавам с това. Проблемът е, че често в резултат на сериозно претоварване с тежести се появява доста неприятна и продължителна болка в кръста и врата. Видях реклама на Лежанките и реших да пробвам, бях опитвал какво ли не – инжекции, лекарства, масажи и нищо не помагаше. С Лежанката трябва да кажа,… Read more „Фитнес ООД“
Клиентите ни обикновено са хора, които искат да поддържат добра форма и тонус, но последно време при нас идват и клиенти със сериозни болки от неврологични заболявания, на които препоръчахме инверсна лежанка. Мой роднини бяха ползвали продукта при проблеми с дискова херния и ошипяване на гръбнака и при тях имаше доста бърз ефект. Затова започнах да препоръчвам лежанката и на мои клиенти… Read more „Уога Днес ЕООД“
Искам да напиша няколко реда за Лежанки и се надявам моят опит да е полезен на хората, които от години се борят с коварната дископатия. Занимавах се професионално с художествена гимнастика още от дете и след близо 12 години професионален опит, започнаха моите кошмари с болките в гърба , врата и кръста. Знам, че дисковата херния като цяло се проявява при хора… Read more „Михаела Цветкова“
От години имам проблем с дископатия, която се опитвах да преборя по много различни начини – тренировки, упражнения, лекарства и нищо не ми помагаше. От близо 2 години страдат от сковаваща болка в кръста, причинена от дископатия. Преди няколко месеца прочетох някъде за инверсните лежанки Teeter. Имах съмнения, бях пробвам доста неща, но нищо не помогна. Доставиха ми лежанката вкъщи… Read more „Излекувах се!“
Поръчахме продукти от каталога за целия офис. На този етап мога да кажа, че получихме изключително положителни коментари и хората са много доволни от упражненията и твърдят, че след работа се чувстват по-здрави, вместо по-уморени. Мисля, че уредите имат страхотно приложение за офиса и дори ги считаме за вид забавление, освен основната им полза за здравето. Препоръчвам за всякакви… Read more „Препоръчвам за офиси“
Първо купих лежанка за себе си. После препоръчах на сестра ми. После заедно подарихме на майка ни. Сега препоръчваме на всичките ни други роднини и приятели. Много по-малко напрежение изпитваме в гърба и въпреки че изглеждат големи, изобщо не заема място… Read more „Препоръчах на всички роднини“
Обожавам туризма и пътуванията още от малък. Почти всеки месец съм в друг град, друга държава, и държа да обиколя всички забележителности. Преди около половин година ми се появиха болки в гърба, като всеки лекар имаше различна теория, но най-често го свързваха с дългото ходене. Излишно е да споменавам, че нищо не помогна, а това да се тъпчеш с лекарства… Read more „По-добре от лекарства“
Единственото, което искам да споделя, е да не отлагате като мен! Няколко месеца умувах дали да си поръчам подобна лежанка, а болките продължаваха. Когато най-сетне го направих, почувствах леко облекчение още през първата седмица и ефектът продължаваше да се подобрява през следващите. Не чакайте, тези лежанки са… Read more „Заслужава си“
Само можем да се присъединим към мнението на хората, които препоръчват тези лежанки. Шефовете купиха такива за офиса и отначало повече ги възприемахме за шега, когато някой виси надолу с главата. Месец по-късно на всички сутрешната им тренировка е в офиса и само си споделяме истории кой колко по-добре е започнал да се чувства. Така че… не го мислете много,… Read more „С колежките сме много доволни“
Просто искам да споделя опит, че от всички сайтове и доставчици, с които разговарях, от Lejanki бяха най-любезни, най-бързи и за мен лично са най-изгодното място, откъдето да си намерите подобни… Read more „Най-изгодни са офертите в Lejanki“
Тези лежанки са чудесен избор за дома, употребяват се много бързо и лесно, като цената им не е нещо особено за добрите резултати, които постигат. Препоръчвам за покупка за дома на хора, които искат да водят по-здравословен начин на живот, но имат заето… Read more „Бързо, лесно, изгодно“
През първите дни не помня да е имало особена разлика, може и да съм си въобразявал. След 1-2 седмици чувствах гърба си като след кратък масаж или тренировка (когато добавях и малко загряване преди разтягането). Месец по-късно определено е видно, че имам по-малко напрежение в гърба и болката вече отшумява. Няма да спра да ги… Read more „Добри резултати след 1 месец“
Изпробвала съм и други лечения, масажи и терапии, като парите никак не са били малко. Основната разлика между Ember и останалото, което изброих, е, че тук инвестицията е еднократна, след това го правите вкъщи и отнема 10-15 минути. Всъщност, си… Read more „В крайна сметка, излиза по-евтино“
Искам само да изкажа своята благодарност за бързата и точна доставка, успях да се справя сам със сглобяването за 15 минути и вече я пробвах – чудесен… Read more „Перфектна доставка“
За по-малко от 30 минути ми доставиха и сглобиха лежанката, без да губя и минута от своето време. Сега й се радвам във всекидневната и от 1 седмица я използвам всеки… Read more „Качествена доставка, сглобяват на място“
За хора като мен, които стоят пред компютър по 14 часа на ден, лежанките на Ember се оказаха изключително попадение! Не съжалявам, че ги поръчах, даже напротив. Ползвам ги близо месец и половина, по 1 час на ден и определено нямам досегашното схващане и скованост във врата и кръста. Радвам се, че ви открих и поръчах от… Read more „За хора като мен“
Гледах доста клипчета в Ютуб, четох много за лежанките на Ember преди да се реша да си поръчам. От години страдам от стеноза и нямаше постоянно облекчение много време нито от инжекции, нито от физиотерапия, до операция няма да стигам. Та да се върна на лежанките. Ползвам ги от месец, не съм ползвал нито гелове, нито хапчета, само тях. И… Read more „Лежанките са супер! Препоръчвам ги горещо.“
Всеки, който страда от болки в гърба, особено от години, трябва да има уреда вкъщи. При мен болките в долната част на гърба бяха станали неразделна част от живота ми – ставам боли ме, ходя на работа – боли ме, лягам – боли ме. Нищо не беше в състояние да подобри състоянието ми. Пробвал съм билки, мазила, персонални тренировки, физиотерапия..… Read more „Хора, продукта наистина действа!!!“
